The science of pendemics Of course. The term you’re referring to is Pandemic Science. It’s not a single discipline but a vast, interconnected field that studies the emergence, spread, impact, and control of pandemics. The science of pandemics, often called pandemic preparedness and response, draws from numerous scientific fields to understand and combat global disease outbreaks. Here’s a breakdown of the key scientific disciplines involved:
Virology & Microbiology
- This is the foundation. Scientists in these fields study the pathogens themselves.
- Identification: Isolating and identifying the novel virus (e.g., SARS-CoV-2) or bacteria causing the outbreak.
- Characterization: Understanding its structure, genetics, how it enters cells, and how it replicates.
- Evolution: Tracking mutations and the emergence of new variants.
- Pathogenesis: Studying how the pathogen causes disease in the human body.
Epidemiology
- Surveillance: Tracking cases, hospitalizations, and deaths to map the spread.
- Transmission Dynamics: Determining how the disease spreads (e.g., airborne, droplets, surface contact), and calculating critical metrics like the R0 (R-naught) or basic reproduction number.
- Identifying Risk Factors: Determining who is most at risk (e.g., by age, occupation, pre-existing conditions) and where hotspots are emerging.
Immunology
- This field studies the immune system’s response to the pathogen.
- Antibody Response: Understanding how the body fights the infection and whether prior infection confers immunity.
- Vaccinology: The development of vaccines, which train the immune system to recognize and fight the pathogen without having to get the disease first. This was spectacularly demonstrated with the rapid development of mRNA and other COVID-19 vaccines.
- Severe Disease: Understanding why some people have severe immune responses (like cytokine storms) while others have mild or no symptoms.
Public Health & Medicine
This is the application of science to protect communities and treat individuals.
- Non-Pharmaceutical Interventions (NPIs): Recommending and evaluating the effectiveness of measures like mask-wearing, social distancing, lockdowns, and hand hygiene.
- Clinical Management: Developing treatment protocols, repurposing existing drugs, and creating new therapeutics (e.g., antivirals like Paxlovid).
- Healthcare System Capacity: Managing ICU beds, ventilators, and staff to prevent hospitals from being overwhelmed.
Data Science, Modeling, and Bioinformatics
Modern pandemics are fought with data and algorithms.
- Predictive Modeling: Creating complex models to forecast case numbers, hospitalizations, and the potential impact of various intervention strategies. This helps leaders make informed decisions.
- Genomic Sequencing: Using technology to sequence the genome of the virus from thousands of patient samples. This allows scientists to track variants in near real-time and see how the virus is spreading and evolving across the globe.
- Data Dashboards: Aggregating and visualizing data for the public and officials (e.g., the Johns Hopkins COVID-19 dashboard).
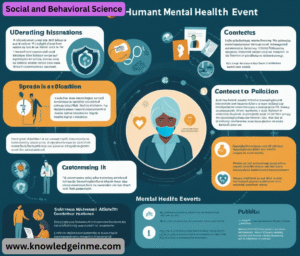
Social and Behavioral Science
- A pandemic is a biological event that occurs within a social context. Understanding human behavior is crucial.
- Risk Communication: Crafting clear, consistent, and effective public health messaging to encourage protective behaviors.
- Addressing Misinformation: Studying how misinformation spreads and developing strategies to counter it.
- Understanding Compliance: Determining why people do or do not follow public health guidelines, and designing strategies to improve adherence.
- Mental Health Impact: Studying the effects of isolation, fear, and grief on population mental health.
One Health Approach
- A critical modern concept recognizing that human health is intimately connected to the health of animals and our shared environment.
- Zoonotic Spillover: Most emerging infectious diseases (e.g., COVID-19, Ebola, Avian Flu) originate in animals. “One Health” focuses on monitoring animal populations, understanding the ecological and environmental pressures (like deforestation and wildlife trade) that lead to spillover events, and preventing them.
The Pandemic “Lifecycle”
Pandemic science operates across a continuous cycle:
- Preparedness: (During peacetime) Building surveillance systems, stockpiling PPE, planning protocols, and researching platform technologies (like mRNA).
- Detection & Early Response: (Spark) Identifying a novel pathogen early and trying to contain it before it becomes a pandemic.
- Containment & Mitigation: (Spread) Implementing public health measures to “flatten the curve” and reduce the burden on healthcare systems while vaccines and treatments are developed.
- Treatment & Vaccination: (Tools) Ramping up the production and equitable distribution of medical countermeasures.
- Recovery & Learning: (Aftermath) Rebuilding societies and analyzing the response to improve preparedness for the next inevitable pandemic.
Advanced and Interconnected Concepts
- The real complexity emerges at the intersection of these fields. Here are some critical advanced topics:
The Science of Superspreading:
- Not all infected individuals spread the disease equally. Pandemic science heavily studies superspreading events.
- Dynamics: These are situations where a single individual infects a disproportionately large number of people. This is often due to a combination of viral load, timing of shedding, behavior (e.g., talking loudly, singing), and environment (e.g., poorly ventilated, crowded indoor spaces).
- Implication: This understanding shifts the focus from just limiting overall contacts to specifically avoiding high-risk environments. It explains why, for instance, closing crowded bars can be more effective than blanket lockdowns.
Genetic Sequencing & Phylodynamics:
- This is the “DNA detective” work that transformed pandemic response during COVID-19.
- How it works: Scientists sequence the genome of the virus taken from thousands of patient swabs. Every time the virus replicates, it makes small mistakes (mutations).
- Tracking Spread: By comparing these genetic sequences, scientists can build a family tree for the virus. This allows them to see how it is moving from one country to another, or if an outbreak in a city is coming from a single source or multiple independent introductions.
- Variant Tracking: This is how variants like Delta and Omicron were identified, tracked, and assessed for properties like increased transmissibility or immune evasion.
The R Value and Beyond:
- While the Basic Reproduction Number (R0) is famous, epidemiologists use more nuanced measures:
- Effective Reproduction Number (Rt): This is R0 in real-time. It measures the average number of people infected by a single person at a specific time, t, in a population where some people may already be immune. An Rt below 1 indicates an outbreak is shrinking.
- Heterogeneity: As mentioned with superspreading, the distribution of spread is just as important as the average. Some people cause many cases, while others cause none.
Modeling the Storm:
- Models are not crystal balls; they are sophisticated “what-if” simulators.
- Types: There are compartmental models (like the SIR model – Susceptible, Infected, Recovered) and agent-based models (which simulate the actions of millions of individual “agents” in a virtual society).
- Purpose: They are used to compare scenarios. For example: “What is the difference in total hospitalizations if we open schools on Monday versus if we wait two weeks?”
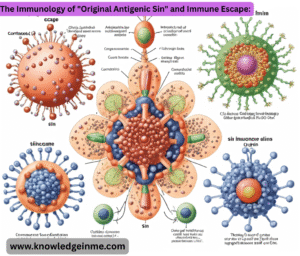
The Immunology of “Original Antigenic Sin” and Immune Escape:
- This is a complex immunological concept crucial for understanding viruses like influenza and SARS-CoV-2 that evolve.
- Original Antigenic Sin: The tendency of the immune system to rely on the memory of a past infection when faced with a similar but new variant, sometimes making the response to the new variant less effective.
- Immune Escape: This is when mutations in a virus variant (often in the spike protein) allow it to partially or fully evade the immunity generated by previous infection or vaccination. This is the primary driver behind updated vaccine boosters.
Major Challenges and Ethical Dilemmas
Pandemic science operates under immense pressure and involves difficult trade-offs.
- The Speed of Science vs. Certainty: Normally, science is slow, cautious, and relies on peer review. Pre-print servers (publishing papers before full review) became vital for sharing information quickly, but also risked spreading unvetted findings.
- Trade-offs of NPIs: Lockdowns save lives from COVID but can increase deaths from despair, delay cancer screenings, and devastate economies.
- The distribution of those vaccines was not. This created a moral and epidemiological crisis: allowing the virus to rip through unvaccinated populations anywhere increases the risk of new variants emerging everywhere.
- Science communication struggled to combat false narratives, often because clear, simple messages (“wear a mask”) had to be updated as the science evolved (“now wear a better mask”), which was exploited to erode public trust.
The Future of Pandemic Science
The goal is to move from reactive response to proactive preparedness.
- Universal Vaccines: A major focus is developing a “universal” vaccine against coronaviruses or influenza viruses that would target conserved parts of the virus, making it effective against all current and future variants, preventing a pandemic from starting.
- Global Early Warning System: Building a robust “One Health” surveillance network that continuously monitors viruses in animal populations (e.g., bats, birds) and in humans at the human-animal interface to detect potential pandemic viruses before they spread widely.
- AI and Digital Surveillance: Using artificial intelligence to analyze vast datasets—from genetic sequences to travel patterns to social media reports of illness—to predict and detect outbreaks faster than ever before.